- Details
- Hits: 5966
- Details
- Hits: 6084
By R Carter
The American Medical Association estimated in 2008 there were 41,718 practicing anesthesiologist, by 2019 that number had dropped to 29,030 according to sources other than the AMA. Primary Care Physicians (PCPs) treated roughly 52% of the 30-50 million chronic pain patients prior to 2010, by some estimates as many as 60% of those PCP’s no longer treat chronic pain, requiring, at a conservative estimate,18 million patients to either look elsewhere or have no access to medical care at all.
To a great extent this decline is a result of cracking down on providers who prescribe opioids for chronic pain, that crack down coming from medical boards and law enforcement.
Another estimate I’ve read says that for every physician no longer treating chronic pain, as many as 300 patients no longer have access to medical care. While no firm estimates exist for these kinds of criteria, the number of patients without access to medical care for chronic pain is still easily in the millions.
This response is due to the false and misleading narritive that treating chronic pain is the leading cause for opioid addiction and overdoses. When overdoses continued to climb after 2013 and as prescribing dropped nationwide as lmuch as 35%, the narrative changed. Now it was an (IMF) problem or illegally manufactured fentanyl.
But there are facts which health officials and government failed to report. These entities didn’t begin testing for IMF on a large scale until 2014, meaning overdose deaths from IMF could have been going on for years and they’d never known it, all along pointing a finger at prescribing as the problem. As more doctors were indicted and jailed for over prescribing, under this false narrative, the news media became hyper-focused on these reports and the topic went viral. This is what you call going off halfcocked, or as I call it premature adjudication.
Prior to 2014 law enforcement crime labs and toxicology testing by coroners, did not routinely test for types of opioids other than heroin, morphine, hydrocodone and oxycodone; using a $2 reagent strip. Identification of IMF required the more expensive gas chromatography and mass spectroscopy, at a cost of several hundred dollars per test, state governments were not about to fund such tests on a large scale for crime labs or coroners offices.
Unable to consider other alternatives as the cause for the opioid deaths, there was no ability to connect the dots between prescribing and overdose deaths. This rush to judgement and to adjudicate, has produced the results we see today. Law suits against pharmaceutical companies, physician associations which promoted active pain management as the 5th vital sign and yes physicians losing their license for doing what they had been doing, some for as long as forty years. The only difference between then and now was the fact that more patients were dying of opioid overdose. Based on data showing an increase in the number of prescriptions written during this time and surveys done on individuals coming out of drug trestment centers, health officilas assume the two were connected. Ignoring the fact that on a per patient basis, the amounts prescribing to individuals hadn’t really changed to any significant degree during the same time frame. So why did people start suddenly dying? No one ever stopped long enough to check for other drug sources, nor was an large scale effort made to correlate the identities of OD deaths with individuals who had been prescribed an opioid for pain.
In a large part, the tools, procedures and funding didn't exit for this type of 1:1 matching of OD victims to prescriptions, that is until Prescription Drug Monitoring Programs were implemented in the early 2010 - 2011 time frame. Health officials reported to government what they assumed to be the cause, because they had no other means to say oterhwise. The idea that illegal drug traffickers may be producing and distributing IMF never occured, the thinking was, drug trafficers were too dumb to make something like IMF, so no one ever bothered to test for it.Once testing begain in 2014 on a large scale, the number of OD deaths from IMF sky rocketed.
The other important piece to pinning down which substances were driving OD deaths was the manner in which public health officals and coroners account for the types of opioids. Knowing the most OD deaths involve multple drugs, sometime as many as six, our system for accounting did not require identification of the primary substance that caused the OD death. Such test again require the more expensive chromatography and mass spectroscopy, testing for the specific types of substances as well as the quantities in the individuals system at the time of death.
Operating on an assumption, because the means didn't exit for connecting the dots, millions of chronic pain patients are now suffering and hundreds if not thousands of doctors have lost their license to prescribe, practice or they’ve been jailed based on these assumption; which at best, are only half true. Were some prescribers exploiting patients, to addict them for profit, yes. Were others possibly too liberal in the amounts they prescribe, perhaps. Were some prescribers cutting corners, failing to perform random urine drug screens, or rushing through exams because insurance reimburstment rates were so low that a $60-90 payment barely covered the cost of performing an hour long examine the associated tests? Yes!
But such missteps don't account for patients who choose to turn to street drugs because they are cheaper and easier to obtain that going to a doctor. Prescribers have no control over what a patient does after they leave the office. A random urine drug screen done once every 2 or 3 months is not likely to pickup on a patient abusing 4 or 5 other drugs on an occasional basis, nor is it guarunteed to identify IMF.
States have had prescription drug monitoring programs (PDMP’s) for at least 10 years now, and that data could easily be used to confirm or deny the extent to which prescribed opioids contribute to overdose deaths. It's a fair assumption to say that all States are performing these comparisons now, but States will not publish this data. What are those comparisons showing and why are they hiding it?
This poll of sixty questions on state medical boards, physician practice and law enforcement, with regards to chronic pain management and the prescribing of opioids, was open to any visitors coming to CERGM. In all 812 individuals started the poll but only 466 completed it. Most left the poll when asked to confirm their identity with an email address which prevents multiple responses from the same individual.
The poll collected general demographic data such as gender, age group and home state but was primarily directed at two groups, patients and healthcare professionals. Most graphs will display results from these two groups so the reader can compare results.
With regards to treating chronic pain, views on medical boards and targeted elements of physician practice, both healthcare professionals and patients had similar views and opinions. On the subject of opioid use disorder those similarities disappeared, with responses spread out nearly even between all available answers. The conclusion seems to indicates that personal experience and beliefs continue to carry more weight than known facts regarding OUD. As such OUD continues to be as misunderstood among healthcare providers as it is among the general public. This remains a major concern, for as long as the public and healthcare providers see OUD and chronic pain management as on in the same, the chronic pain patient (CPP) will continue to be treated first as an addict and second as a legitamate pain patient.
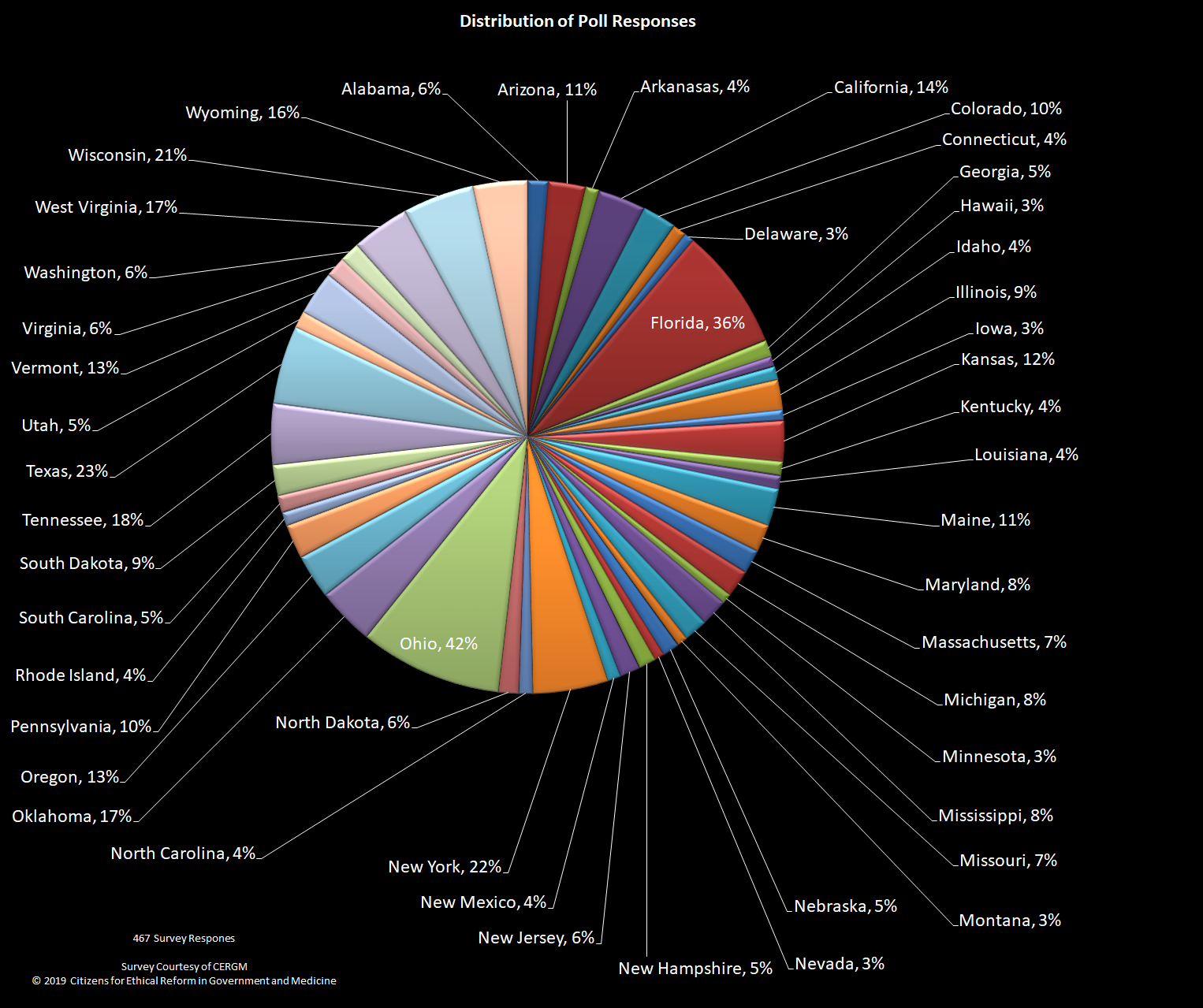
Because of the number of questions, groups and topics, the results for this poll will be published in three parts. Poll results were checked for multiple entries from the same individual and when duplicates occurred, any unfinished survey was deleted and completed results were kept. Of the 466 completed results all but one of the fifty US states is represented, with the largest groups coming from Ohio at 42% and Florida at 36%.
Some charts have a lot of data, such as the one below showing the percentage of individuals from each state. Each chart can be downloaded or clicked on to open it in a separate window for easier viewing.
Demographics of poll group
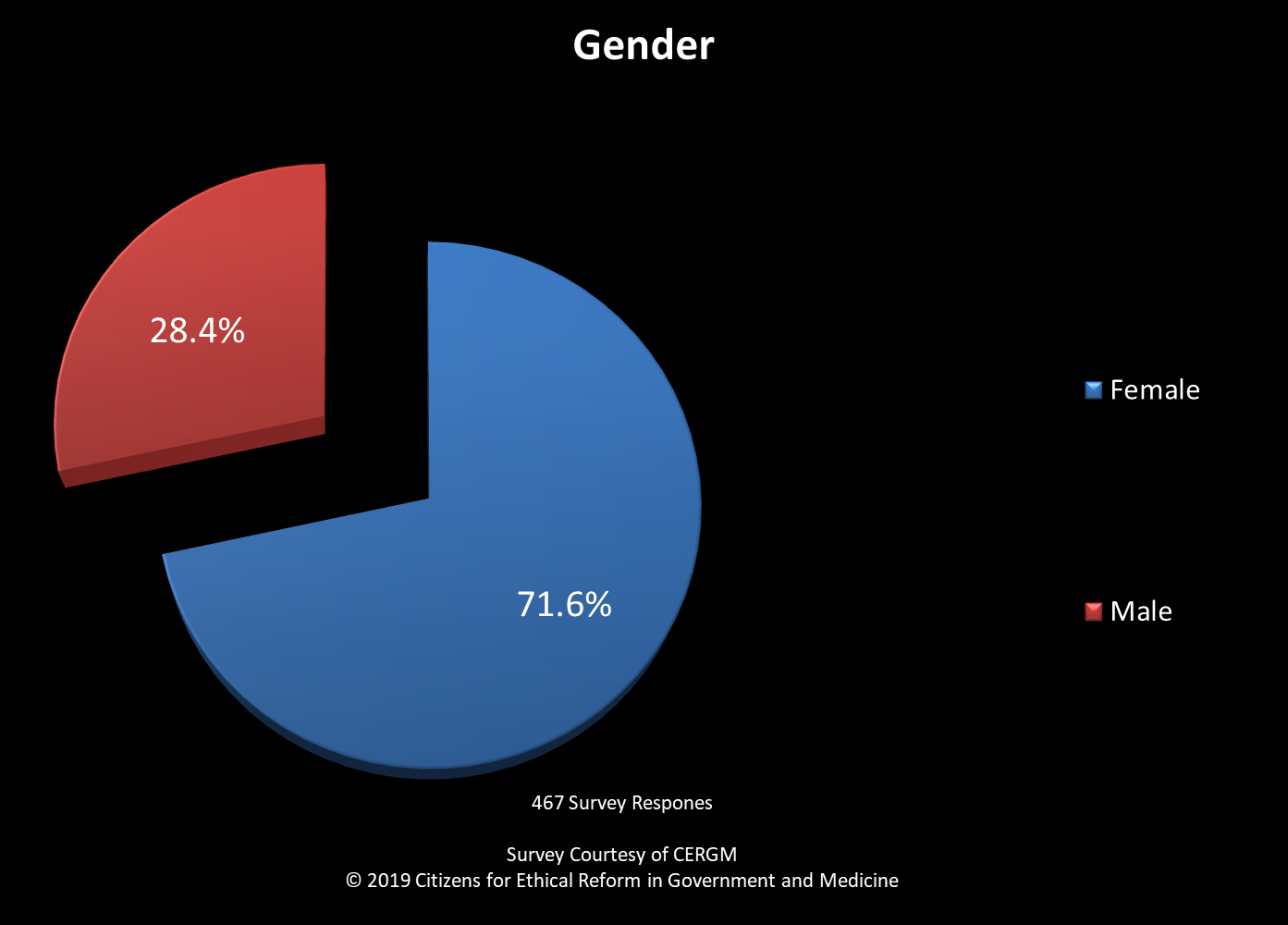
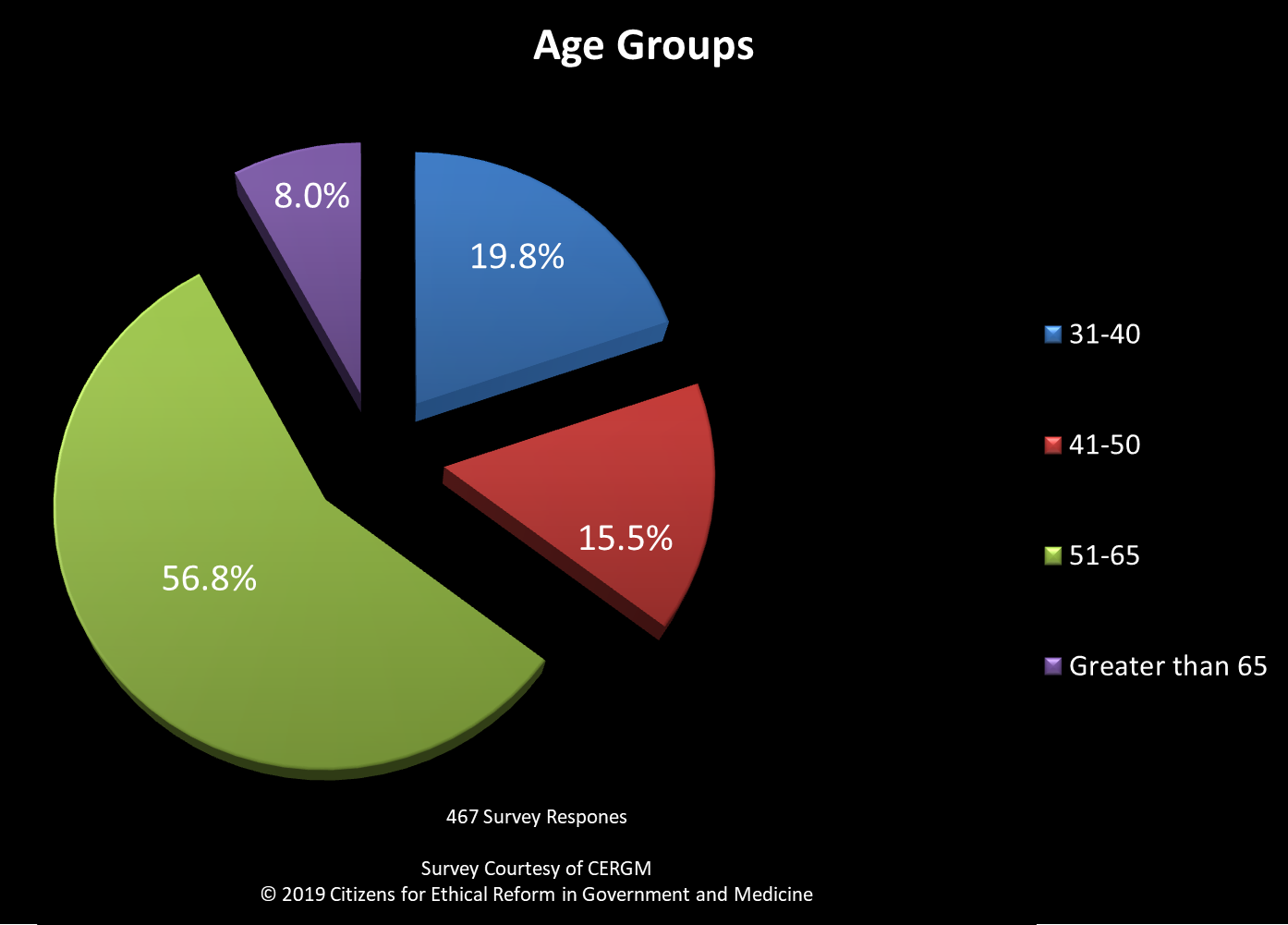
Women out numbered men by 3:1 and respondents, age 50 and above, were the largest by age group which has consistently been the case on polls done at this sight, see Figures 2 and 3.
Participants were asked are they currently or in the past, been a practicing healthcare professiona or a non-professional working with pain patients in some capacity. Between these three groupings 130 out of 466 or 27.8% of respondents had professional experience in healthcare. Another 28.6% or 133 were non-professionals having at least a casual knowledge and some experience about healthcare issues surrounding chronic pain management. See Figures 4-6.
- Details
- Hits: 60273
Your donations allow us to protect the doctor-patient relationship.
DPF Support Package
Our new Support Package includes the following items:
- 10 printed DPF Brochures
- 1 DPF Cup
- 1 DPF Pen
If you would like to receive this package as a thank you for your donation of $50 or more, please use the donate link. In the field where you can write an optional note, please let us know you'd like the DPF Support Package. Please include your name and address in the note, also. Thank you!
 |








